Massachusetts General Hospital Department of Surgery
Center for Artificial Intelligence & Innovation Research
At the Center for Artificial Intelligence & Innovation Research (CAIIRE), our mission is to transform healthcare by harnessing the power of artificial intelligence, driving innovative research, and promoting access to novel technologies.

About the Center
The Massachusetts General Hospital Center for Artificial Intelligence & Innovation Research (CAIIRE) is a multidisciplinary group of doctors, engineers, researchers working together to innovate patient care. Our team harnesses the power of Artificial Intelligence (AI) to lead cutting-edge research across five key focus areas.

Prediction of Postoperative Complications
Our team is developing algorithms that use biometric data from personal wearable devices to predict postoperative complications after major operations. Currently, there is a major gap in patient monitoring in the weeks following hospital discharge – a time when patients remain at high-risk for post-operative complications. As we move into a new era in which wearable devices are becoming ubiquitous, wearable tools that proactively alert patients and providers about complications prior to symptom onset can play a transformative role in improving patient outcomes.

Cancer Risk Prediction
While lung cancer screening with a low-dose computed tomography (CT) scan is the best way to detect lung cancer early, many high-risk patients remain ineligible for lung cancer screening. Notably, there are major racial and sex-based disparities in lung cancer screening eligibility. A team led by MGH faculty members Dr. Lecia Sequist, Dr. Florian Fintelmann, and MIT researcher Dr. Regina Barzilay developed Sybil, an AI tool that can improve early lung cancer detection. Sybil is a 3-D convolutional neural network that examines an entire chest CT scan and estimates probabilities that lung cancer will be diagnosed in each of the next six years.

Computer Vision for Intra-operative Surgical Analysis
We are developing computer vision algorithms to automatically analyze and interpret videos of operations as they are occurring. Our goal is to train AI to understand what is happening during operations, in real-time. In the future, we strive to develop computer-vision based tools to support intra-operative decisions and identify patients who are at high-risk for postoperative complications. Additionally, we hope to develop computer-vision based tools to improve education of surgical trainees.

Virtual Reality Interventions for Pain Management
Our team is developing strategies to combine virtual reality (VR) and olfactory stimulation to improve patient sleep, pain, anxiety, and sleep quality while in the hospital. Patients in our pilot study are offered an intervention consisting of an immersive audiovisual VR experience displaying jellyfish pulsing at 40 beats per minute (half of that average heart rate) accompanied by aquatic white noise and heart sounds. The VR experience is paired with a lavender olfactory stimulus (OS). At night, patients are provided with a sleeping mask infused with the same OS. We hypothesize, based on preliminary research from collaborator Dr. Judith Amores, that the overnight OS may trigger memory reactivation of the relaxing VR experience, and resultantly reduce pain, lower anxiety, and improve sleep quality.
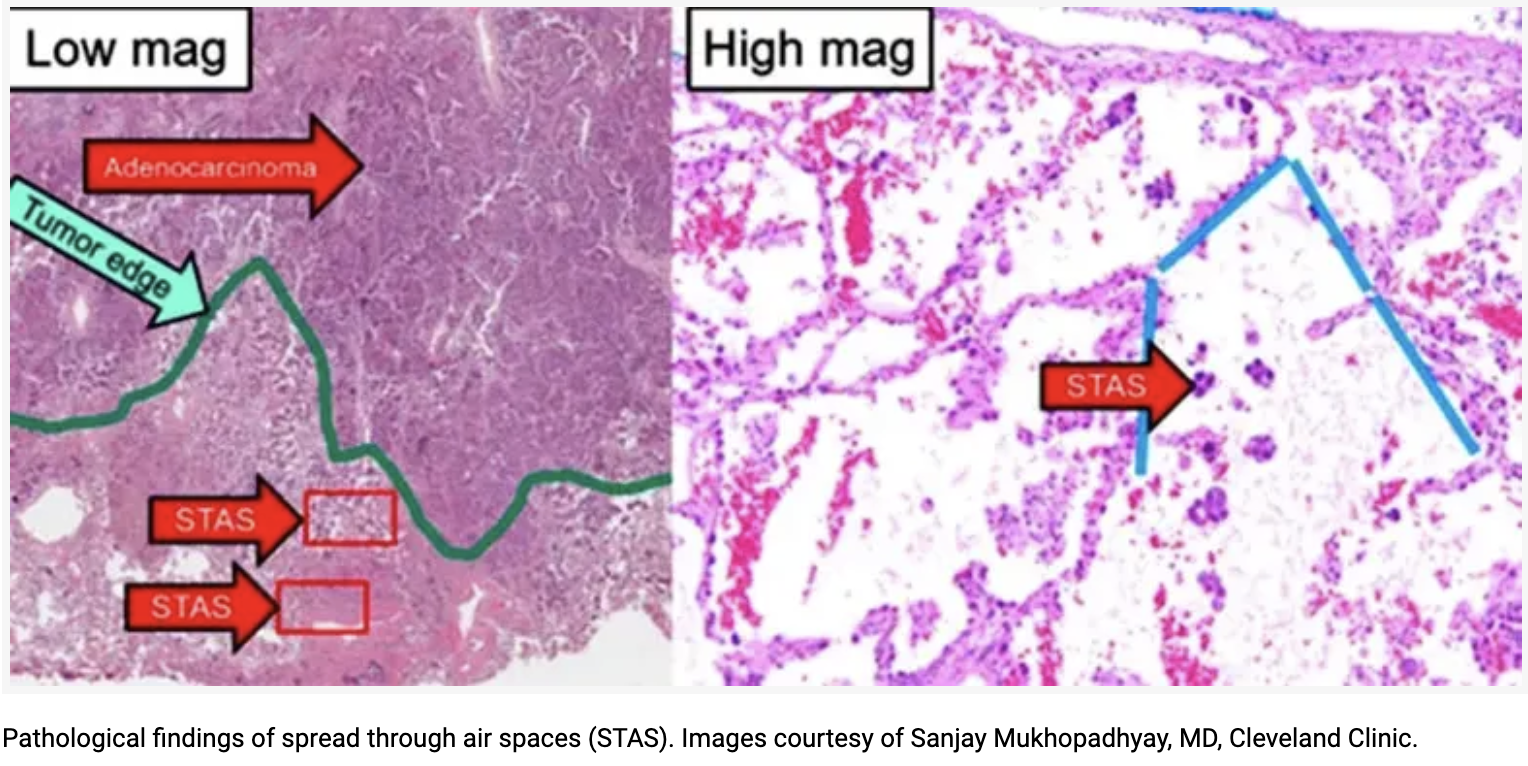
Computer Vision to Predict Lung Cancer Spread Through Air Spaces
Spread through air spaces (STAS) is a unique phenomenon in lung cancer that was recently recognized by the WHO in 2015. It is believed that invasion of airspace may be associated with worse recurrence-free and overall survival, but there has so far been no reliable way of identifying potential STAS in the pre-operative setting. We are working to identify clinical and radiomic factors associated with STAS and develop a combined computer-vision based clinical radiomic model to predict STAS status pre-operatively.
Meet our Center
Director

Chi-Fu Jeffrey Yang, MD
Dr. Chi-Fu Jeffrey Yang is a thoracic surgeon at Massachusetts General Hospital, an Associate Professor of Surgery at Harvard Medical School, and the Founding Director of the Center for Artificial Intelligence & Innovation Research (CAIIRE). He practices all aspects of thoracic surgery, including procedures for conditions of the lung and mediastinum. He specializes in minimally invasive techniques. Dr. Yang has received numerous awards, including recognition for exceptional accomplishment in both clinical care and in teaching. In 2021, he received the Harvard Medical School Charles McCabe Faculty Prize for Excellence in Teaching. In 2024, he received the Clifton F. Mountain Lectureship Award for Staging from the International Association for the Study of Lung Cancer. He is a member of the American Association for Thoracic Surgery and the Society of University Surgeons.
Learn more
Dr. Yang leads several clinical studies. He is co-principal investigator and project leader of a $3.5 million NIH R01-funded study evaluating postoperative complications and recovery in cardiothoracic patients. He is also the co-principal investigator and project leader of a $1.5 million AHRQ R18-funded lung cancer screening study. Dr. Yang serves as Vice Chair of the Alliance Thoracic Surgery Group. Dr. Yang has been the lead or senior author on several high impact papers published in the JAMA, British Medical Journal, Journal of Clinical Oncology, JAMA Oncology, Lancet Respiratory Medicine, Journal of Thoracic Oncology, Annals of Surgery, and Chest. He has written over 160 publications, including over 90 as first-, co-first or senior author. Dr. Yang is an editorial board member of the Journal of Thoracic and Cardiovascular Surgery, the Journal of Thoracic Diseases, and the Society of Thoracic Surgeons Online Curriculum. He is also an associate editor for Pearson’s General Thoracic Surgery.
Meet the Program
Director

Arian Mansur, BA
Arian Mansur is a fourth-year medical student at Harvard Medical School interested in specializing in cardiothoracic surgery.
Arian received his bachelor’s degree in Human Developmental and Regenerative Biology with a secondary in Global Health and Health Policy from Harvard University, where he graduated Magna cum laude with Highest Honors in the field.
Arian’s research focus is on transforming surgery with the help of artificial intelligence. He is also actively engaged in conducting clinical research on patient outcomes, quality of care, and surgical education. Arian has presented his work in several national conferences and has been the lead author on several high impact papers published in Chest, Annals of Thoracic Surgery, and the Journal of Thoracic and Cardiovascular Surgery.
Meet the Program
Coordinator

Soneesh Kothagundla
Soneesh Kothagundla performs clinical research at Massachusetts General Hospital. His research focuses on the applications of artificial intelligence (AI) in medicine.
Soneesh has a deep passion for investigating how AI can improve the early detection of diseases and patient outcomes. A key focus of his research is in using AI to identify individuals at risk for lung cancer who are eligible for lung cancer screening. Soneesh also focuses on studying the use of AI to improve patient outcomes after major surgery. In addition, Soneesh is the leader of several large-scale initiatives with the American Lung Cancer Screening Initiative, a 501(c)(3) non-profit that aims to increase access to lung cancer screening.